February 3, 2015
Blurb
Widespread Dopamine Deficits Found in Brains of Patients with Schizophrenia
VIDEO: https://www.youtube.com/watch?v=_F2saRo_yHw&feature=youtu.be
New York, NY(February 4, 2015) – Columbia researchers have found evidence of reduced levels of the transmitter dopamine in the frontal cortex of patients with schizophrenia. This deficit, which affects the ability of the frontal cortex to become activated when the subjects are faced with cognitive demands such as memory tasks, is most likely responsible for the cognitive deficits that patients with schizophrenia suffer from. The study was published online on February 4, 2015, in JAMA Psychiatry.
This dopamine deficit in the frontal cortex is in contrast to the excess dopamine that researchers have found in the striatum, a region deep inside the brain. That excess produces the hallucinations, delusions, and thought disorder associated with psychosis.
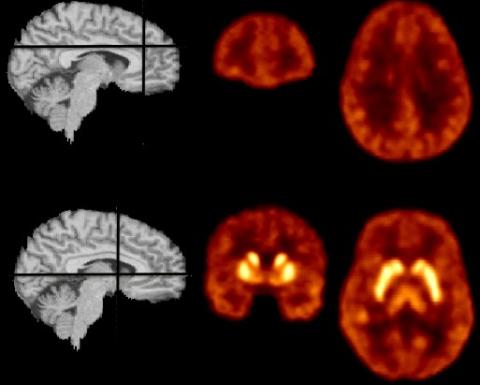
Until now, it has been difficult to examine dopamine in the cortex, where the neurotransmitter is essential for cognition: remembering for brief intervals of time, reasoning, strategizing, and other related functions. Using PET imaging technology, first author Mark Slifstein, PhD, and colleagues compared dopamine activity in the frontal cortex in patients with schizophrenia and in healthy controls. They found that patients with schizophrenia have lower levels of dopamine in the frontal cortex.
“We also found that in patients with schizophrenia, most of the brain regions that we could image with this imaging tool have deficits in dopamine,” said Dr. Slifstein, associate professor of neurobiology (in psychiatry) at Columbia University Medical Center (CUMC) and research scientist at the New York State Psychiatric Institute.
Though researchers had suspected for a long time that the abnormal dopamine activity associated with schizophrenia was not limited to the striatum, the current study is the first to demonstrate the extent of the dysfunction.
“Recognizing the presence of cortical deficits in dopamine helps us to understand why current treatments fail to address cognitive problems and negative symptoms, which are at least partly mediated by dopamine transmission in some of these brain regions,” said principal investigator Anissa Abi-Dargham, MD, professor of psychiatry at CUMC and Chief of the Division of Translational Imaging at the New York State Psychiatric. “Furthermore, the information enables us to search for specific disease mechanisms and helps guide treatment developments.”
The title of the paper is, “Deficits in Prefrontal Cortical and Extrastriatal Dopamine Release in Schizophrenia: A Position Emission Tomographic Functional Magnetic Resonance Imaging Study.”
See paper for the complete list of contributors.
This research was funded by grant 1 P50 MH066171-01A1 from the National Institute of Mental Health to Dr. Anissa Abi-Dargham, and the Sylvio O. Conte Center for the Study of Dopamine Dysfunction in Schizophrenia.
Dr. Slifstein has received research support from Forest Laboratories, Pierre-Fabre, CHDI, and Otsuka and has provided consultation for Agmen. Dr. Narendran has received research support from Ono Pharmaceuticals Co Ltd. Dr. Girgis has received research support from Otsuka and Genentech. Dr. D’Souza has received research support from AbbVie and Pfizer and has provided consultation for Bristol Myers Squibb, and Johnson and Johnson. Dr. Lieberman has received research support from Biomarin, EnVivo, Genentech, Novartis, Psychogenics, and Eli Lilly and has served on advisory boards for EnVivo, Intracellular Therapies, Pear Therapeutics, and Pierre Fabre. Dr. Lieberman also has a patent with Repligen. Dr. Abi-Dargham has received research support from Takeda and Forest Pharmaceuticals and has served on advisory boards for Roche, Forum, and Otsuka. No other disclosures were reported.
####
Columbia University Department of Psychiatry and New York State Psychiatric Institute (Columbia Psychiatry/NYSPI)
New York State Psychiatric Institute (founded in 1896) and the Columbia University Department of Psychiatry have been closely affiliated since 1925. Their co-location in a New York State facility on the NewYork-Presbyterian/Columbia University Medical Center campus provides the setting for a rich and productive collaborative relationship among scientists and physicians in a variety of disciplines. Columbia Psychiatry/NYSPI are ranked among the best departments and psychiatric research facilities in the nation and have contributed greatly to the understanding of and current treatment for psychiatric disorders. The Department and Institute are home to distinguished clinicians and researchers noted for their clinical and research advances in the diagnosis and treatment of depression, suicide, schizophrenia, bipolar and anxiety disorders, and childhood psychiatric disorders. Their combined expertise provides state-of-the-art clinical care for patients and training for the next generation of psychiatrists and psychiatric researchers.
Visit http://nyspi.org and http://columbiapsychiatry.org/ for more information.
